I think it's one of those questions where you know the answer, but really don't know the answer, because you know the reason why we do attenuation correction (AC), but really don't know how it is applied on our patients. Thus the question, "how does attenuation correction work?"
To start, the principles of AC applies to both SPECT/CT and PET/CT alike, even though we are using different isotopes and energy levels for these systems.
The CT unit is the main equipment piece that helps us to make this work. The reason why is, it is the x-ray's that shoot through the body, which gets collected by the CT detector array on the other side that provides the AC data.... "but we know that already!". The problem lies in the fact that the x-rays and the energy of the isotopes are different. Let's use Tc-99m as an example. The problem is this, how do you use a 70 keV x-ray to correct for the nuclear medicine SPECT scan if the energy level for acquisition is at 140 keV? These energies interact and attenuate differently as it traverses through the body!
When the x-rays are produced from the x-ray tube, there are a spectrum of low to high energies generally, where low energy x-rays get absorbed by the tissues whereas the high energy x-rays pass right through the body, if it is used unfiltered. This is something that we do not want because it makes it harder to figure out the AC maps. Thus the x-rays are filtered (wedge or bow tie) to produce an average of 70 keV's to help simplify the process. The process isn't perfect, but it "hardens" the beam to eliminate the "ends" of the x-ray spectrum.
 |
| Fig. 2 The the x-rays are filtered to help simplify the process of AC. |
Once we collect the x-ray data from the detectors, the information is reprocessed. The most important piece of information is the linear attenuation coefficient (u), which is calculated by using this formula, aka Beer's Law:
 |
| Formula taken from CT1 course, CAMRT |
The little (u) can now be used to calculate the CT numbers to differentiate the different densities in the body based on the Hounsfield unit scale on our display monitors.
So the question now is, "How do we put all this information together to understand AC?!?!"
We've acquired our CT and what you see are whole bunch of CT numbers converted to the Hounsfield's scale, based on the (u) values of the CT x-rays. The next step is to convert this data and create a correction factor for the corresponding voxels in the SPECT scan. To do this, we need to calculate the new (u) value that is scaled to 140 keV. Basically, what would be the new (u) value if we converted 70 keV x-ray to 140 keV (the Tc-99m energy that we want to scale it to)?
There's two parts to this scaling:
1. Formulas to calculate and scale the 70 keV to 140 keV based on the original CT number acquired for your CT scan
2. A bilinear graph (model) used to convert CT numbers to (u) values for specific radionuclides like Tc-99m, In-111, Ga-67, F-18 etc.
The formulas:
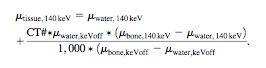 |
| Fig.3 Top: Formula for (u) for CT values less than 0 (0 being water). Bottom: Formula for (u) for CT values greater than 0. These are bit hard to see, but look them up in this article: SPECT/CT Physical Principles and Attenuation Correction |
The bilinear graph, works hand in hand with the formulas, because it just gives a graphical overview of how the CT numbers are treated when the CT values are below or above CT=0. The reason for the bilinear graph is to account for the different densities in the body (ie. water and air mix OR water, soft tissue and bone mix).




This seems so simple.
ReplyDeleteWell done!
ReplyDelete